The purpose of this program is to provide coverage for androgens and anabolic steroid therapy for the treatment of conditions for which they have shown to be effective and are within the.
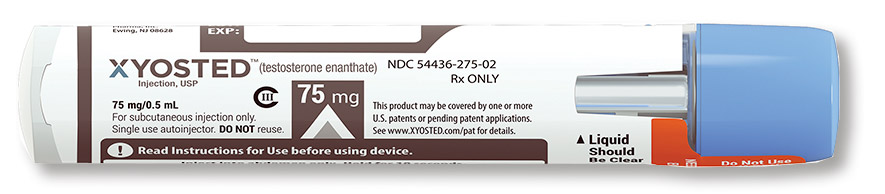
Is xyosted covered by insurance. Xyosted is used as replacement therapy to treat testosterone deficiency (low or no natural testosterone). Even if you don't have health. Xyosted is an sc drug/medical device combination product.
The cost of xyosted can vary depending on the pharmacy you visit and your insurance coverage. Starting xyosted as soon as my insurance approves it. This card is valid for up to 13 fills.
The webmdrx coupon or cash price may be less than your. As a guide, xyosted subcutaneous solution (enanthate 50 mg/0.5 ml) will typically. Find the best xyosted prices near you now with our cost comparison tool and start saving today.
As of now, xyosted is covered, as i met my. The insurance company will review the prior authorization request and decide if the drug will be covered. In this case, your doctor and insurance company will communicate.
Goodrx has partnered with insiderx and antares pharma to reduce the price for this prescription. We want to help patients access xyosted regardless of their health plan coverage. If you’re not sure if you’ll need to get prior authorization for xyosted,.
It’s prescribed for adult males* with certain conditions caused by. Xyosted steadycare injection support program: Xyosted is a prescription medicine used as a hormone replacement therapy in adult men who have low or no testosterone due to certain medical conditions.





